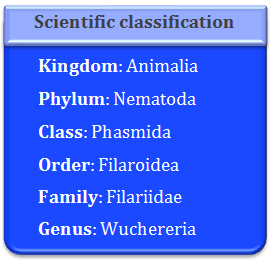
Wuchereria bancrofti is commonly called as the filarial worm, as it causes the disease filariasis, in human beings. The larval form of this worm was discovered by Demarquay. Later Wucherer found these larvae in the chylorous urine. Lewis found them in human blood. Bancrofti found them in adult females. This worm is named after two scientists Bancroft and Wucherer.
It is pseudocoelomate round worm. It requires a blood sucking vector for its transmission as its larvae. Microfilariae are present in the blood capillaries of human beings. Sir Patrick Manson discovered that female culex mosquitoes are the vectors for this parasite.
Common names: Wuchereria bancrofti is also called as Bancrofti worm, Elephantiasis worm, Filariasis worm
Distribution: Filariasis worm is worldwide or cosmopolitan in distribution except at Polar Regions. It is more common in tropical regions like Arabia, India, Malaya, Korea, China, Japan and Brazil. It is almost absent in Europe, North America and African continents.
Habit and Habitat: Wuchereria bancrofti is a dangerous human parasite found in human blood and lymph. It is a digenetic parasite and it requires two hosts to complete its life cycle. The two hosts are man and female culex mosquito. The adult worms are harbored in a coiled state in human lymph glands and lymph passage. These worms obstruct the passage of the lymph.
Identification: Adult worms are cylindrical in shape. They are creamy white in color. The male and female sexes are separate and they exhibit sexual dimorphism.
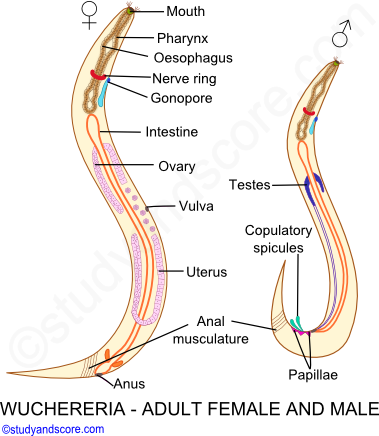
The female worms are slightly longer and thicker than that of their male counterparts. Female worms measure 65 to 100 mm in length and 0.25 mm in diameter whereas male worms measure 40 mm in length and 0.2 mm in diameter. The posterior end of the female worms is sharply curved with genital papillae, while the posterior end of the male not much curved.
The anterior ends of these worms terminate bluntly whereas the posterior end is a little pointed. The male and female worms are found coiled round each other in the lymph vessels and thus block the flow of lymph and this results in the enlargement of the concerned organ.
A mouth with no oral lips is present at the anterior end. The alimentary canal of this worm includes mouth, pharynx, oesophagus, intestine and anus. The anterior part of the pharynx is muscular and the posterior part is glandular.
The posterior end of the female is straight and bears anus. The female genital pore called vulva is present ventrally at about one third length of the body from the anterior tip. The posterior end of the male worm is curved bearing cloaca. A pair of unequal copulatory spicules is present in cloacal region. Many copulatory papillae are present in the posterior region.
There are 8 filarial species with humans as definitive hosts. They are tabulated hereunder:
| Filarial Parasite | Location | Disease |
|---|---|---|
| Wuchereria bancrofti | Lymphatics | Elephantiasis |
| Burgia malayi | Lymphatics | Elephantiasis |
| Burgia timori | Lymphatics | Elephantiasis |
| Loa loa | Eye subcutaneous | Kalabar swelling |
| Onchocerca volvulus | Subcutaneous | Onchocercomata |
| Mansonella perstans | Abdominal cavity | Mild Allergy |
| Mansonella ozzardi | Body cavity | Mild Allergy |
| Mansonella streptocerca | Subcutaneous fat | Mild Allergy |
Wuchereria is a heterogeneous parasite which completes its life cycle in two different hosts namely man and female culex mosquito.
Life cycle in Man: Human Phase
Copulation takes place in Human lymphatic system. Male and female worms copulate when they are present in the same lymph gland. The female worms are ovoviviparous and produce eggs which hatch within the body of the female without obtaining nourishment from it. Numerous microscopic juvenile larvae called microfilariae are released into the lymph.
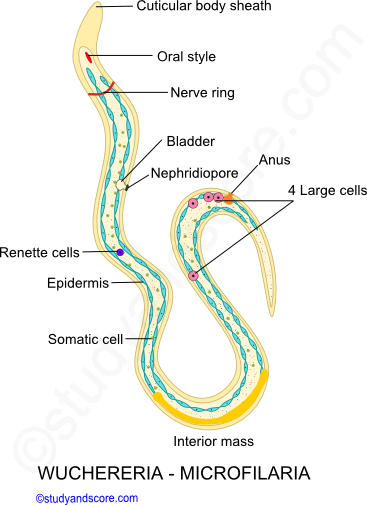
Each microfilaria is about 0.2 to 0.3 mm in length and is surrounded by loose cuticular sheath, also known as egg membrane. The surface of this larva is covered by flattened epidermal cells. Its body contains columns of cytoplasm with a number of nuclei. An oral style is present at the anterior end where the mouth develops in future. Microfilaria also bears the following parts,
The microfilaria after being released into the lymph vessels, enter the blood vessels and circulate with the blood. Ultimately they migrate to the visceral organs and reside in deeper blood vessels of thorax region. In this thorax region the larvae do not undergo any additional change as further development can happen only inside the intermediate host.
Thus, these larvae move to the peripheral blood vessels during the night time, to suit the feeding habit of mosquito. During the day time these larvae live in large deep-seated blood vessels but during night they migrate to the peripheral blood vessels. This movement of the larvae is called as nocturnal periodicity or diurnal rhythm. The microfilariae die if they are not transferred to the mosquito within 70 days. Microfilaria is the infective stage to mosquitoes.
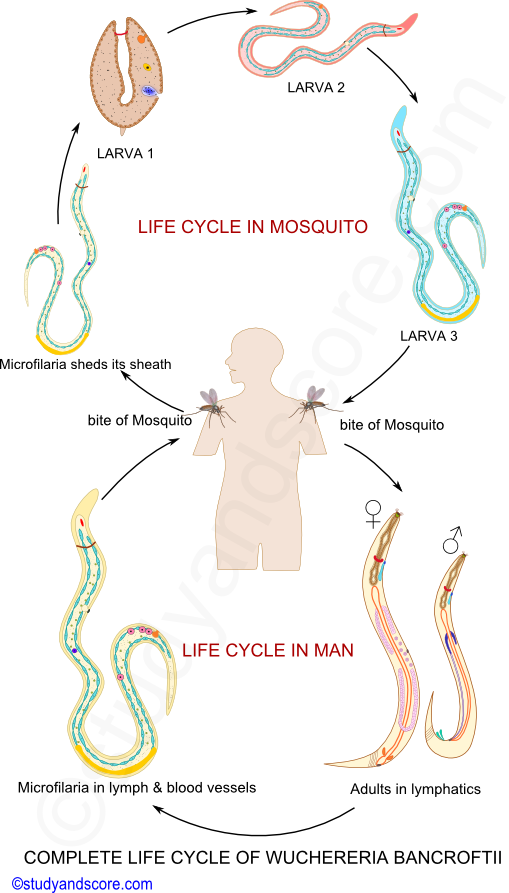
Life cycle in Mosquito: Mosquito Phase
When the female Culex quinquefasciatus mosquito sucks the blood from the Wuchereria-infected person, the microfilaria from the peripheral blood, enter the midgut of the mosquito. In the midgut they shed their protective sheath within 6 hours. They penetrate the stomach wall and migrate to the thoracic muscles where they metamorphosis and grow.
Initially they metamorphose into a flat sausage-shaped larva also called as first-stage larva. Later this larva undergoes first moulting and grows into a slender elongated second-stage larva. Finally this second stage larva undergoes second moulting transforming into a long infective stage also called as the third-stage larva. All these changes take place within 10-20 days. The final third-stage larva moves to the labium of the mosquito so that it can be transferred to man.
In man the filarial larva first enters the blood circulation through the bite of the mosquito and then it enters into the lymphatic vessels where it undergoes third and fourth moulting and transforms into adult. The adult male and female worms copulate and the female delivers microfilariae.
Lymphatic Filariasis (LF) also called as filariasis or elephantiasis, renders the patient with severe weakness and disability. It imposes social and economic burden to the affected individuals as well as their families. Lymphatic filariasis is an obstacle to socioeconomic development.
LF is the world’s second leading cause of long-term disability in the affected patients. The current estimate reveals that globally 120 million people are infected with lymphatic filarial parasites and about 20% of the world’s population is at risk of getting infected. According to the World Health Organization, India, Indonesia, Nigeria and Bangladesh alone contribute about 70% of the infection.
Filariasis in India
In 6th century BC Susruta recorded this disease, elephantiasis in his book ‘Susruta Samhita’ and in 7th century AD, Madhavakara described signs and symptoms of this disease in his work ‘Madhava Nidhana’. In 1709, Clarke named elephantoid legs in Cochin, Kerala as ‘Malabar legs’. For the first time, in 1872, Lewis discovered microfilariae in the peripheral blood.
Indigenous lymphatic filariasis cases are reported from 21 States and Union territories like Andhra Pradesh, Assam, Bihar, Chhattisgarh, Goa, Gujarat, Jharkhand, Karnataka, Kerala, Madhya Pradesh, Maharashtra, Orissa, Tamil Nadu, Telangana, Uttar Pradesh, West Bengal, Puducherry, Andaman & Nicobar Islands, Daman & Diu, Lakshadweep and Dadra & Nagar Haveli.
The North-Western States like Jammu & Kashmir, Himachal Pradesh, Punjab, Haryana, Chandigarh, Rajasthan, Delhi, Uttaranchal and North-Eastern States like Sikkim, Arunachal Pradesh, Nagaland, Meghalaya, Mizoram, Manipur and Tripura are known to be free from indigenously acquired filarial infection, owing to the variations in the temperatures.
Control and elimination of Filariasis in India
National Filaria Control Programme, launched in 1955 has a three dimensional approach to curb filarial infections. The strategies include in this programme are
The World Health Assembly resolution (1997) has targeted to eliminate filariasis by 2020, whereas India’s National Health policy envisaged elimination of filariasis by the year 2015. But this target is missed out and currently as many as 35 crore people in 13 states continue to remain under the risk of filarial infection. Odisha, UP, Bihar, West Bengal, Jharkhand and Chhattisgarh are the states at extremely high risk.
The Union health ministry has prepared the National Roadmap for Elimination of Lymphatic Filariasis (NRELF) with clear goals, objectives, strategies, timelines with activities and functions at appropriate level to achieve the target.
The current elimination strategy is based on two pillars that is annual mass drug administration with Diethylcarbamazine (DEC) along with albendazole for five years or more to the population excluding children below two years, pregnant women and seriously ill persons in affected areas to interrupt transmission of the disease.
Eliminating filaria in India is a big public health success story after receiving polio-free certification. Currently India is reaching elimination targets with the increase in population coverage during mass drug administration and decrease in overall microfilaria rate at the national level.
- Share with your friends! -
Login to post your comment here...
- or with social Account -